Comprehensive Guide to Blood Test Consent Legislation in the UK
Understanding the Intricacies of Legal Consent Requirements

The legal framework governing blood test consent laws in the United Kingdom is complex and essential, encompassing a wide array of legal statutes and regulations that are designed to protect individual rights. Key legislation, such as the Mental Capacity Act 2005, highlights the necessity of obtaining informed consent from individuals who may lack the mental capacity to make educated choices. The Human Tissue Act 2004 specifically regulates the collection and use of human tissues, including blood, for medical purposes. Additionally, the Data Protection Act 2018 plays a crucial role in how personal data—including medical information related to blood tests—is handled. Collectively, these laws establish a comprehensive framework that guarantees consent is informed, voluntary, and specific, thereby safeguarding patient rights and ensuring the integrity of medical practices.
- Mental Capacity Act 2005
- Human Tissue Act 2004
- Data Protection Act 2018
- General Medical Council (GMC) Guidelines
- Health and Social Care Act 2008
- Common Law on Informed Consent
- Care Quality Commission (CQC) Regulations
- National Health Service (NHS) Constitution
Who Is Legally Empowered to Provide Consent for Blood Tests?
In the United Kingdom, the authority to grant consent for a blood test predominantly rests with the patient themselves, provided they possess the mental capacity to comprehend the implications of the test. This typically applies to adults aged 18 and above; however, special provisions are in place for minors and individuals who may be deemed to lack mental capacity. For minors, the responsibility for consent generally falls to parents or guardians, yet adolescents aged 16 and over may independently consent to their own medical treatment under certain conditions, as guided by the Gillick competence principle. Should an individual be assessed as unable to provide consent due to mental incapacity, the Mental Capacity Act mandates that any decisions made must prioritise the individual's best interests, taking into account their previously expressed wishes and feelings, thus respecting their autonomy.
What Are the Consequences of Failing to Obtain Consent?
Neglecting to secure proper consent before conducting a blood test can result in severe repercussions, both legally and medically. From a legal standpoint, healthcare practitioners may be faced with allegations of battery or negligence, which could lead to disciplinary actions or legal claims against them. Medically, patients who feel that their consent has not been respected may refuse treatment altogether, which can adversely affect their health outcomes and diminish their trust in the healthcare system. The potential outcomes of failing to obtain consent may include:
- Legal actions against healthcare professionals
- Disciplinary proceedings initiated by regulatory bodies
- Increased patient distrust in medical practitioners
- Liability for damages sought in civil court
- Health complications stemming from delayed diagnoses
- Risk of reputational damage to healthcare institutions
- Negative repercussions on future patient consent processes
- Possible criminal charges for assault
How Is Adherence to Blood Test Consent Laws Monitored and Maintained?

The Crucial Responsibilities of Healthcare Providers in Securing Consent
Healthcare providers, including doctors and nurses, carry significant responsibility for ensuring that consent is obtained and accurately documented prior to performing blood tests. Their obligations encompass clearly articulating the nature and purpose of the test, discussing associated risks, and presenting any alternative options available to the patient. Consent should not merely be viewed as a signature on a form; it represents a dynamic process where patients are actively engaged and fully informed. Essential responsibilities in this context include:
- Providing clear and comprehensive information about the blood test
- Ensuring that the patient fully understands the implications of their consent
- Accurately documenting consent in the patient’s medical records
- Effectively assessing the patient’s capacity to consent
- Respecting the patient’s right to withdraw consent at any time
- Training staff on legal requirements concerning consent
- Implementing tailored policies for minors and individuals with mental incapacity
- Addressing any queries or concerns from the patient regarding the test
How Is Compliance with Blood Test Consent Laws Monitored Effectively?
Compliance with blood test consent laws is rigorously monitored through various regulatory frameworks established within the UK healthcare system. The Care Quality Commission (CQC) plays a pivotal role in overseeing healthcare providers to ensure that quality standards, including those related to consent procedures, are met. Regular inspections and audits are carried out to assess whether consent is properly obtained and documented. Furthermore, healthcare institutions frequently maintain internal compliance teams tasked with ensuring adherence to the General Medical Council (GMC) guidelines pertaining to consent. Continuous professional development and regular training sessions for healthcare staff are also essential in upholding compliance with these laws, fostering a culture of accountability and awareness.
What Are the Consequences of Violating Consent Laws?
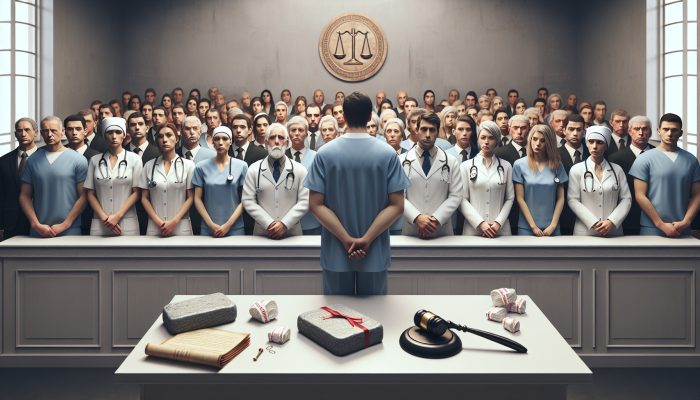
When consent laws are violated, the repercussions for healthcare providers can be severe. Breaching consent protocols may trigger formal investigations by regulatory bodies such as the General Medical Council or the Nursing and Midwifery Council. Potential outcomes could include legal actions, such as civil lawsuits for negligence or breaches of duty. Practitioners may also face disciplinary actions, including suspension or removal from their professional registers. Furthermore, violations can lead to healthcare institutions incurring fines, suffering reputational damage, and losing public trust, which can adversely affect the quality of patient care provided.
Expert Insights on Blood Test Consent Regulations
Case Studies Demonstrating the Application of Consent Laws
A recent case at a London hospital highlights the strict enforcement of consent laws, where a patient successfully challenged the validity of a blood test conducted without proper informed consent. This incident prompted a thorough review of the hospital’s consent protocols, reinforcing the critical necessity of adhering to consent laws in healthcare settings. Such real-life examples underscore the importance for healthcare providers to implement robust and transparent consent processes, ultimately protecting patient rights and nurturing trust within the healthcare system.
Concrete Strategies for Healthcare Professionals to Ensure Compliance
Healthcare professionals can significantly bolster adherence to blood test consent laws by creating standardised consent forms, holding regular training sessions focused on consent protocols, and establishing clear communication channels with patients regarding their rights and options concerning blood tests. By cultivating an environment where patients feel informed and empowered to make decisions regarding their healthcare, professionals can markedly enhance the overall quality of patient interactions and preserve the integrity of the consent process.
What Challenges Do Healthcare Providers Face When Implementing Consent Laws?
Healthcare providers frequently encounter a range of challenges in implementing blood test consent laws, particularly in acute care environments where time constraints necessitate swift decision-making. Assessing mental capacity can also prove complex, especially among vulnerable populations requiring additional support. Moreover, the ever-evolving landscape of consent laws presents difficulties in keeping pace with best practices and regulatory requirements, necessitating ongoing training and adaptability among healthcare professionals to ensure compliance while prioritising patient safety.
Critical Scenarios Where Consent Is Essential
Obtaining Consent During Emergency Medical Situations
In emergency medical circumstances, acquiring consent for a blood test can become particularly complicated, especially when patients are unable to communicate due to their medical condition. The Mental Capacity Act permits the assumption of implied consent in life-threatening scenarios where immediate medical intervention is crucial to save a life. Nonetheless, healthcare providers must still operate within the legal and ethical frameworks established by law, ensuring that any actions taken thereafter align with the patient's best interests, thereby fulfilling their duty of care.
Consent Protocols for Research and Clinical Trials
When blood tests are part of research studies or clinical trials, the consent process becomes even more detailed and intricate. Participants must receive comprehensive information regarding the nature of the research, potential risks, benefits, and their right to withdraw from the study at any time without facing repercussions. In the UK, the UK Policy Framework for Health and Social Care Research outlines these requirements, ensuring that informed consent is obtained and documented accurately before participation in any research activities, thereby safeguarding participants’ autonomy and rights.
What Are the Consent Regulations for Minors in the UK?
Consent regulations for minors in the UK primarily adhere to the Gillick competence principle, which allows minors aged 16 or over to consent to their own medical treatment, including blood tests, if they demonstrate adequate understanding and intelligence regarding the treatment. For those under 16, parental consent is typically required; however, healthcare professionals must also assess the minor’s ability to comprehend the implications of the test, ensuring that their voice is included in the decision-making process.
Consent Protocols in Mental Health Treatment
The consent protocols for mental health treatment are particularly sensitive, especially when patients may lack the capacity to provide informed consent. Under the Mental Health Act 1983, mental health professionals are required to evaluate whether the patient is capable of making informed decisions regarding their treatment, which includes blood tests. If the patient is deemed incapable, decisions made must prioritise the patient's best interests, considering their previously expressed wishes and the insights of family members or advocates, thereby ensuring ethical standards are upheld.
Recognising Patient Rights Regarding Blood Test Consent
Understanding the Right to Information
Patients possess the fundamental right to receive comprehensive information before consenting to a blood test. This encompasses understanding the purpose of the test, potential risks involved, and the implications of the results. Healthcare providers are legally obligated to ensure that patients are fully informed, facilitating a decision-making process that respects patient autonomy. Clear communication and transparency are vital components of patient rights within the consent framework, highlighting the importance of informed decision-making in healthcare.
Patients’ Right to Decline a Blood Test
The legal right of patients to refuse a blood test is unequivocal and firmly entrenched in UK law. Patients are entitled to decline the test without experiencing coercion or negative repercussions. Nevertheless, healthcare providers must ensure that patients are fully aware of the consequences of their refusal, educating them about the potential health impacts of not undergoing the test, thereby enabling an informed and autonomous decision-making process.
How Can Patients Safeguard Their Rights During the Consent Process?
To ensure that their rights are protected throughout the consent process, patients should engage proactively with healthcare providers, asking pertinent questions about the procedure, associated risks, and potential benefits. Furthermore, patients should feel empowered to express any concerns regarding their treatment, ensuring that their autonomy and preferences are respected throughout their healthcare journey. This proactive engagement not only safeguards their rights but also fosters a collaborative relationship between patients and healthcare professionals.
How Have Blood Test Consent Laws Evolved Over Time?
Examining the Historical Development of Consent Laws
The evolution of blood test consent laws in the UK can be traced back to the landmark Montgomery v Lanarkshire Health Board case in 2015, which significantly altered the legal landscape by placing a stronger emphasis on patient autonomy. Historical advancements include the gradual recognition of the importance of informed consent and the establishment of essential legal frameworks, such as the Mental Capacity Act 2005, which continues to shape current practices surrounding consent in healthcare settings. These legal milestones reflect a growing acknowledgment of patient rights and the necessity for healthcare providers to engage in meaningful dialogues with patients about their care.
Recent Changes and Updates in Consent Legislation
Recent revisions to blood test consent laws have aimed to enhance patient autonomy and better protect vulnerable groups. For instance, the Data Protection Act 2018 introduced stricter guidelines governing the management of personal data, including health information derived from blood tests, ensuring that patients’ rights to privacy and control over their data are maintained. These legislative updates signify a continued commitment to improving the standards of patient care and ethical practices within the healthcare system.
What Future Developments Can Be Anticipated in Consent Laws?
Looking ahead, potential developments in blood test consent legislation may involve a greater integration of digital consent processes, particularly as telemedicine becomes increasingly prevalent. As technology continues to advance, there is potential for legislation to further adapt, addressing ethical dilemmas associated with genetic testing and the implications of artificial intelligence in healthcare decision-making. Such changes could fundamentally transform the consent landscape, necessitating a reevaluation of best practices in obtaining informed consent.
The Influence of Case Law on Blood Test Consent Practices
Significant court rulings have profoundly affected the interpretation and implementation of blood test consent laws. Decisions such as Montgomery have reinforced the necessity for healthcare providers to engage patients in genuine discussions regarding their treatment options, ensuring that consent is not merely a formality but rather an authentic dialogue centred on patient rights and choices. These rulings highlight the evolving nature of consent and the increasing importance of patient engagement in healthcare decision-making.
Evaluating Case Studies and Legal Precedents
Analysing Key Court Cases Related to Consent
One notable case that stands out is Chester v Afshar, which underscored the critical importance of informed consent in surgical procedures. The implications of this ruling extend to blood test consent, reinforcing the necessity for clear communication and understanding between healthcare providers and patients regarding the associated risks and benefits. Such cases illuminate the ongoing dialogue surrounding consent and the responsibilities of healthcare practitioners in enhancing patient understanding.
Significant Rulings Shaping Consent Law
Judicial decisions, including Montgomery v Lanarkshire Health Board, have left an enduring impact on blood test consent practices, establishing a precedent that emphasises the patient’s right to be comprehensively informed about their treatment options. These rulings have shifted the focus from a paternalistic model of healthcare to one that prioritises patient autonomy and informed decision-making, fostering a more collaborative approach to patient care.
What Insights Can Be Derived from These Legal Cases?
From the examination of historical legal cases, it is evident that thorough communication and meticulous documentation are essential components of the consent process. The emphasis on patient autonomy demonstrates that healthcare providers must ensure that consent is not a mere formality; it requires genuine engagement with patients, respecting their rights and preferences in all medical decisions. By learning from these cases, healthcare professionals can enhance their practices and improve the patient experience.
Key Legislation Influencing Blood Test Consent
Significant laws that have shaped blood test consent policies in the UK include the Human Tissue Act 2004 and the Mental Capacity Act 2005. These legislative frameworks have provided a foundation for ethical practices surrounding consent, ensuring robust protections for patients while offering clear guidelines for healthcare professionals in their consent processes. Understanding these laws is crucial for both practitioners and patients navigating the complexities of consent effectively.
Comparative Analysis of Consent Laws Across Various Jurisdictions
When comparing blood test consent laws in the UK to those in other jurisdictions, notable differences arise, particularly concerning approaches to implied consent and patient rights. While the UK places considerable emphasis on informed consent, other countries may operate under different legal frameworks that impact the level of detail required in the consent process or the rights of minors in consent matters. Such comparisons reveal the diversity of legal approaches to consent and underscore the importance of understanding local regulations within a global healthcare context.
Frequently Asked Questions About Blood Test Consent
What is the legal age for providing consent to a blood test in the UK?
In the UK, individuals aged 18 and over can generally provide consent for a blood test. However, those aged 16 and over may consent to their own treatment if they demonstrate sufficient understanding and intelligence regarding the implications of the procedure.
Can a patient refuse a blood test?
Indeed, patients possess the unequivocal legal right to refuse a blood test. Healthcare providers must respect this decision and ensure that patients are fully informed about the implications of their refusal, empowering them to make educated choices regarding their healthcare.
What happens if a patient is unable to consent?
If a patient lacks the capacity to provide consent, the Mental Capacity Act 2005 mandates that any decision made in the best interests of the individual must consider their previously expressed wishes and feelings, thereby ensuring that their autonomy is respected.
Are there specific guidelines for consent in clinical trials?
Yes, participation in clinical trials necessitates detailed informed consent, encompassing information about the trial’s nature, associated risks, potential benefits, and the participant’s right to withdraw from the study at any stage without penalty.
What role does the Care Quality Commission play concerning consent laws?
The Care Quality Commission (CQC) is responsible for monitoring compliance with consent laws among healthcare providers, ensuring that patients’ rights are upheld and that consent procedures are followed appropriately, thereby maintaining standards of care within the healthcare system.
How can healthcare professionals ensure compliance with consent laws?
Healthcare professionals can guarantee compliance by meticulously documenting consent, providing clear and comprehensive information to patients, and participating in regular training sessions focusing on consent protocols, thus fostering a culture of accountability and best practices.
What are the consequences of breaching consent laws?
Breaching consent laws can lead to substantial legal actions, disciplinary measures against healthcare practitioners, and a deterioration of trust between patients and healthcare providers, ultimately resulting in significant consequences for both parties involved.
Do patients have the right to receive information before consenting?
Absolutely, patients have the right to receive thorough information regarding the blood test, including its purpose, potential risks, and implications, ensuring they are well-informed before providing consent.
What does ‘Gillick competence’ refer to?
Gillick competence refers to the legal principle that allows a minor aged 16 or over to consent to their own medical treatment if they can demonstrate adequate understanding and intelligence regarding the treatment, thereby acknowledging their capacity to make informed decisions.
How have blood test consent laws evolved over time?
Blood test consent laws have evolved significantly to emphasise patient autonomy and informed consent, particularly in the wake of landmark cases that have shifted the focus towards a patient-centred approach in healthcare, ensuring that the rights and preferences of individuals are respected.
Connect with us on Facebook!
This Article Was First Found On https://bloodtest.co.uk
The Article Blood Test Consent Laws: Understanding UK Regulations and Rights Was Found On https://limitsofstrategy.com





Comments are closed